Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
Understanding how vaccines work — and how the immune system can better defend you against illness — is an important way you can protect your and your loved ones’ health.
Vaccines help your immune system prevent and fight infectious illness, including invasive pneumococcal disease. This is a group of serious, sometimes life-threatening infections caused by different strains of Streptococcus pneumoniaebacteria. You’ve likely heard of the milder infections caused by this bacteria, such as middle ear infections and sinus infections. But you may not know of the more serious types of pneumococcal disease, such as pneumonia, meningitis (an infection of the lining of the brain and spinal cord) and bacteremia (a bloodstream infection).
“Although invasive pneumococcal diseases are relatively rare, they happen quickly and can kill you within hours or days,” says Mayo Clinic expert and pediatrician Robert M. Jacobson, M.D. “Those at risk cannot afford to depend on their natural immunity to fight these rare infections. This is why vaccination is so critical and so protective, especially for young children and older adults and those with conditions that put them at increased risk.”
Here, Dr. Jacobson talks about exactly how pneumococcal vaccines work, their effectiveness, and why it’s important to follow Centers for Disease Control and Prevention (CDC) pneumococcal vaccine recommendations.
How do pneumococcal vaccines work?
To understand how vaccines work and why they’re necessary, it’s helpful to know some basics about the immune system.
The body has two lines of defense against the germs — including bacteria — that can make you ill. Innate immunity is the body’s nonspecific, “built-in” defenses. The skin, for example, helps keep you healthy by acting as a natural barrier against germs.
The adaptive immune system, on the other hand, has more-targeted defenses. Not only can it identify and attack germs, the adaptive immune system can also “remember” its forays with specific germs. This allows it to fight off germs better and faster when it is exposed to those it recognizes. This adaptive response is why you may have fewer or more-mild symptoms the second time you’re sick with the same illness. In some cases, you may even acquire immunity to a certain condition after getting it once, as with chickenpox.
When it comes to life-threatening and fast-moving infections such as meningitis, Dr. Jacobson says your immune system doesn’t have enough time to learn how to react and build up targeted defenses — leaving you vulnerable to serious illness and even death.
Pneumococcal vaccines are important because they teach your immune system how to target and fight off S. pneumoniaebacteria from the get-go. Put simply, vaccinations give your immune system a “cheat code” against infection.
How does the vaccine interact with the body to prevent disease?
Pneumococcal vaccines work by training the body to identify and react to the presence of specific, disease-causing bacteria.
“Most vaccines use a piece of material that was either made by the disease-causing germ or looks like it was made by the germ,” says Dr. Jacobson. “In general, the pneumococcal bacteria have cell walls made up of sugars. We use these very specific sugars, called polysaccharides, for the vaccines.”
When these materials are introduced into the body by vaccination, white blood cells send antibodies to identify and clean up the foreign substance. Once eliminated, the white blood cells keep watch and remember how to react when the real bacteria come along. As a result, the immune system can ward off infection more effectively. In a way, the vaccine really just creates an effective, well-trained security guard with a knack for remembering trespassers.
What do the different vaccination names mean?
Right now, there are a number of different pneumococcal vaccines available in the United States: the 15-valent pneumococcal conjugate vaccine (PCV15), the 20-valent pneumococcal conjugate vaccine (PCV20), the 21-valent pneumococcal vaccine (PCV21) and the pneumococcal polysaccharide vaccine (PPSV23). The first three are newer vaccines that improve the immune response by affixing a protein to the sugar. The fourth is an older vaccine that lacks the attached protein. The numbers refer to the number of bacterial strains they target.
The CDC recommends pneumococcal vaccination for all children under 5 years old and all adults 65 and older, as their immune systems are more vulnerable to invasive pneumococcal disease. Additionally, vaccination for people with certain chronic conditions — including those who are immunocompromised — is recommended at any age from 5 to 64 years. The exact vaccination type and number depend on a few different factors, including age at vaccination.
If you’re not sure if you’ve been vaccinated or what type of vaccine may be best for you, Dr. Jacobson recommends consulting with your healthcare team.
How well do the vaccines work?
Putting an exact number on the effectiveness of pneumococcal vaccination is a bit tricky, according to Dr. Jacobson, because it depends on the type of vaccine, age and underlying risk factors, time since vaccination, and research data available. For some of the strains, researchers can only estimate effectiveness by examining the amount of antibodies produced by a particular vaccine for a given strain and what is known about the protective level of antibodies for that strain.
Still, the effectiveness of the vaccines has been demonstrated by a reduction in circulating strains and confirmed disease. Research has shown that since the introduction of the newer PCVs in children, the rate of invasive disease has fallen sharply. And it has fallen not just in the children vaccinated but also in adults at risk of infection with the strains contained in the children’s vaccines. This is a form of herd immunity. Since the introduction of PCV13, for example, the rate of infection has fallen by 90% in children. In the past, adults 65 years and older were thought to also need PCV13, but after a few years it became clear that vaccinating just children provides enough herd protection for those 65 years and older. As a result, healthcare professionals stopped vaccinating older adults with PCV13. Until recently, older adults were vaccinated with just PPSV23 to cover strains not included in PCV13. Now with the availability of PCV15, PCV20 and PCV21, older adults and other adults at risk get one of those and, depending on which one, PPSV23 as well. The CDC reports that PPSV23 is 60% to 70% effective against invasive disease in adults.
In short, vaccination is the safest, most effective and most thoroughly tested method to protect yourself and your family from invasive pneumococcal disease, according to Dr. Jacobson. But it is not for everyone. Talk with your healthcare professional to find out if you’re at risk and to get a vaccine recommendation specific to your circumstances.
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
Relevant reading
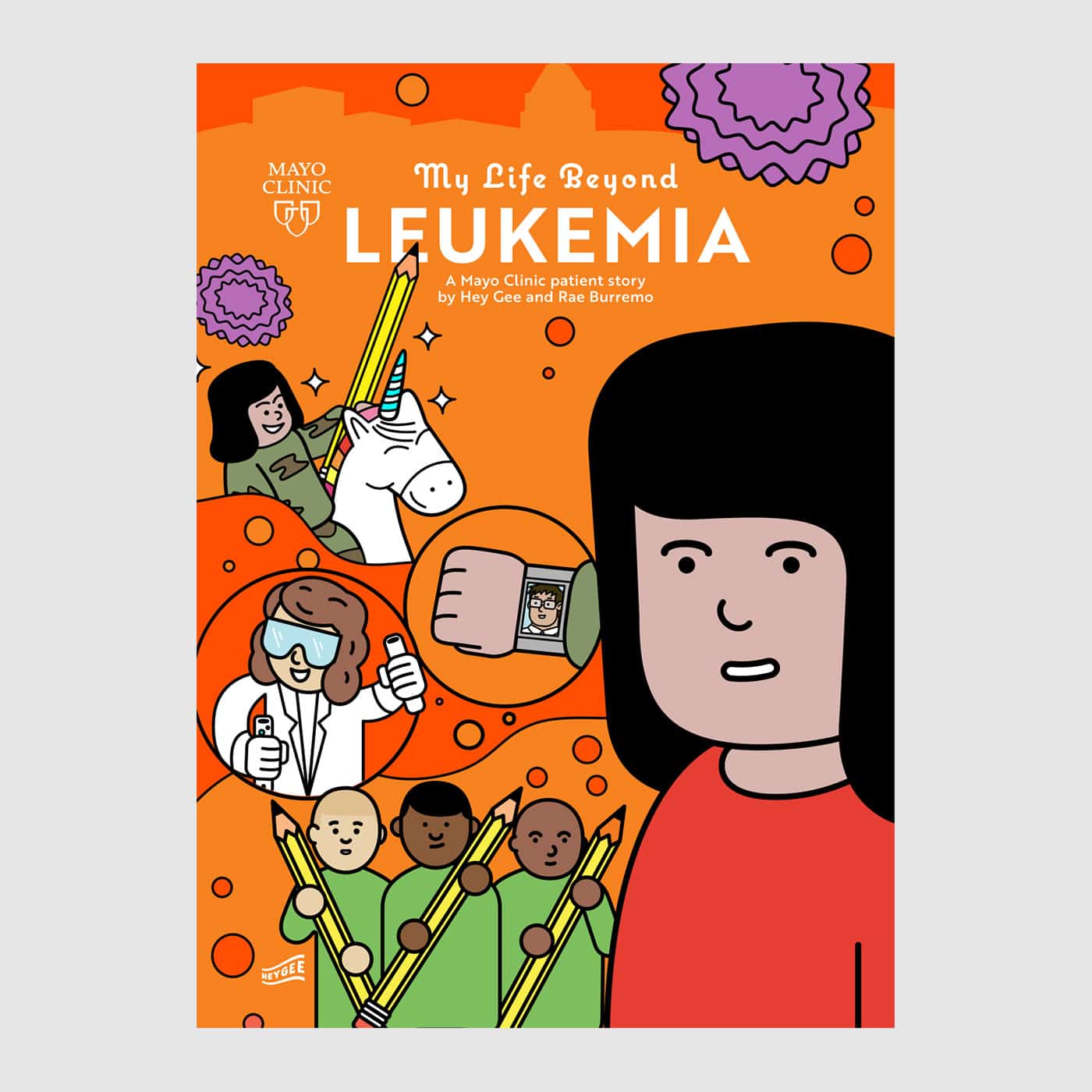
My Life Beyond Leukemia
After going through treatment for leukemia, Amy is used to visiting the hospital. As she falls asleep for another medical test, she suddenly finds herself on an adventure. With the help of a shrinking potion, other magic tools and some friends, she’s on a mission to help other kids face…