Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
With many autoimmune diseases, you need to take medicine for rest of your life.
However, that’s not always true with chronic inflammatory demyelinating polyradiculoneuropathy (CIDP). If you have this condition, your immune system mistakenly targets the myelin sheath that protects the nerves in your arms and legs as foreign, sending out immune cells to attack it. As the protective myelin sheath wears away, you may notice tingling, numbness, weakness and other symptoms.
However, treatment can drive the disease into remission, meaning that ongoing drug therapy may not be necessary.
“The immune system will reset so it doesn’t attack the nerve again, in some cases even after the medicine is stopped,” says Divyanshu Dubey, M.B.B.S., a neurologist specializing in CIDP treatment at Mayo Clinic. “The chances of relapse aren’t zero, but they’re low.”
Once the immune system stops attacking the myelin sheath, nerve tissue heals and symptoms diminish.
“We’ve had patients improve nearly back to how they were before they got the disease,” says Dr. Dubey.
CIDP treatments
The many types of CIDP medicines help stop the immune system from attacking nerves. Specifically, the medicines deplete the cells in the immune system that mark and remember the nerve tissue as foreign, and thus subject to immune attack. Once those immune cells are wiped out, the immune system resets and stops attacking the nerves.
Though full recovery is possible, CIDP can still be tricky to treat. That’s because there are many types of CIDP, and some are more responsive to treatment than others. On top of that, some treatments work effectively for some types of CIDP, but not for others. Treatment methods include the following.
Intravenous immunoglobulin (IVIg)
If you have the more common form of CIDP, your healthcare professional will likely recommend IVIg. This treatment is often delivered in an infusion center.
How it works. Medicine is delivered through a catheter and into a vein. Unlike many medications used to treat autoimmune conditions, IVIg does not suppress your immune system. Instead, it infuses your body with targeted antibodies that help to train your immune system to work correctly.
Eventually, if you respond to treatment, your healthcare professional may switch you to an injectable form of the same medicine that you can administer at home without medical supervision.
What to expect. Your IVIg treatment schedule will vary based on the severity of your symptoms. Initially, many people need four or five infusions a week. Over time, however, as symptoms resolve, you may only need the treatments once every few weeks.
“When started early in the disease for someone with typical CIDP, IVIg can lead to a full recovery,” says Dr. Dubey. “We’ve had few patients become completely symptom-free without any deficits at all.”
Plasma exchange (plasmapheresis)
If your CIDP symptoms are severe, your healthcare professional may recommend that you undergo plasmapheresis.
It’s not a cure for CIDP. However, plasmapheresis is sometimes used to help manage symptoms as people wait for more-permanent treatments like rituximab (Rituxan) or intravenous immunoglobulin to kick in. “It brings about a faster response,” says Dr. Dubey.
How it works. During plasmapheresis, your healthcare professional inserts a needle into your arm. Then your blood travels from your body to a machine, which filters the antibodies from your blood before returning it to your body. The exchange takes several hours.
What to expect. Depending on the severity of your condition, you may need 4 to 7 treatments over 8 to 10 days.
Rituximab (Rituxan)
This treatment tends to work best for people with specific CIDP variants that often don’t respond to IVIg therapy.
How it works. Rituximab is a monoclonal antibody that depletes the immune cells responsible for making antibodies that attack your nerve tissue. Once the medicine has wiped out these antibody-making cells, the immune system resets and stops attacking your nerves.
What to expect. This medication is usually given in six monthly intervals. Therefore, you will visit the infusion center once or twice every six months to receive rituximab. Unlike traditional CIDP, some of the CIDP variants are less responsive to treatment. As a result, your healthcare professional may combine this therapy with plasmapheresis, steroids or other medicines
Other medications
Depending on how your disease responds to treatment, your healthcare professional may pair IVIg or rituximab with other medicines. These include steroid medications to reduce the immune system’s inflammatory response. These second line treatments are generally used only when first line therapies fail to reset the immune system.
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
Relevant reading
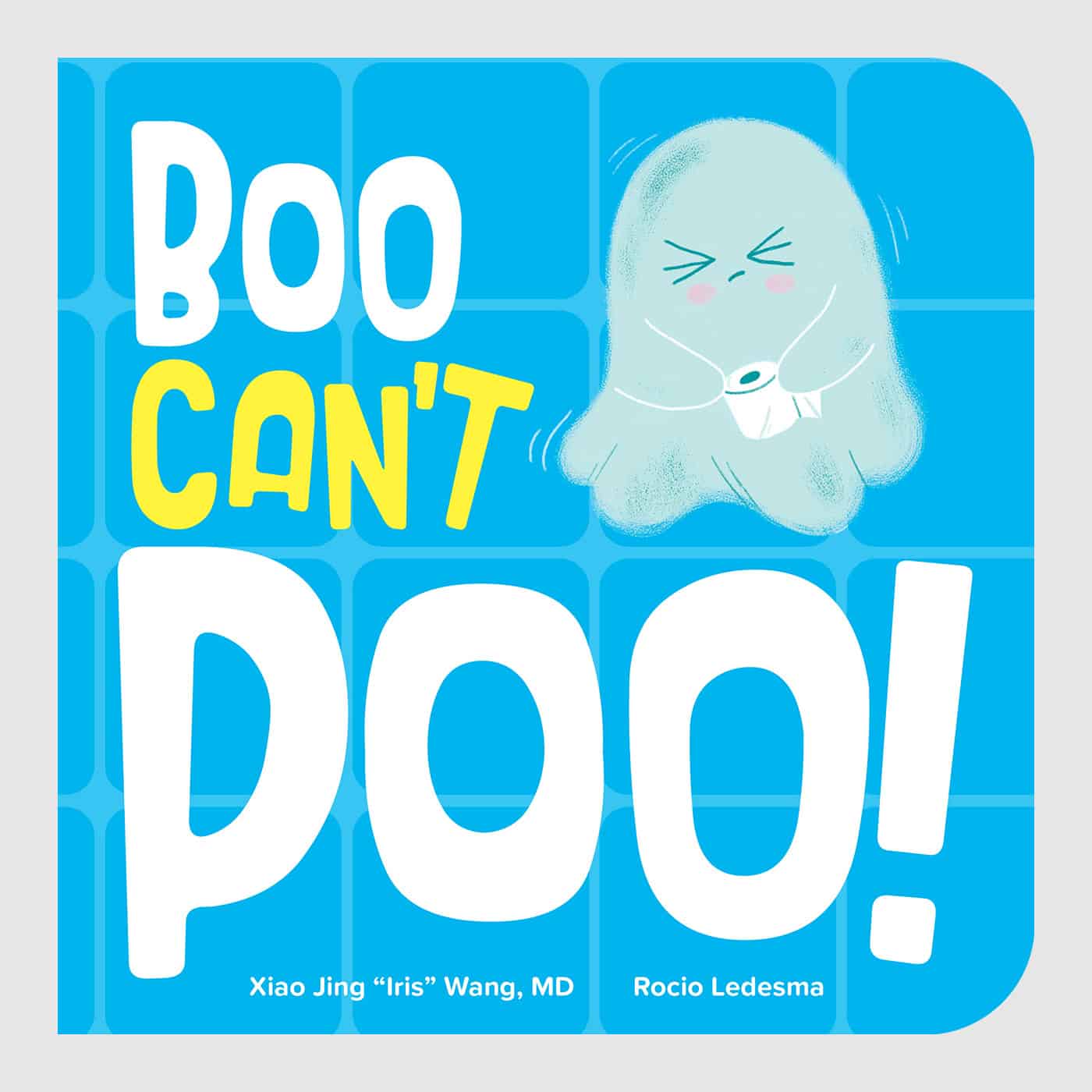
Boo Can't Poo
Get ready to giggle with Boo Can't Poo, the hilarious board book sure to get your little ones laughing and pooping! Join Boo the constipated ghost on his quest to get his bowels moving with the help of his ghostly family. With silly rhymes and cute illustrations, this book is…