Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
Several years ago, the HER2-low breast cancer designation didn’t exist. Tumors were considered to be either HER2 positive or HER2 negative.
So, what is HER2-low breast cancer? More importantly, how does this status affect your treatment plan? Mayo Clinic oncologist Roberto A. Leon-Ferre, M.D., answers some of the most frequently asked questions about HER2-low breast cancer.
What is HER2?
About 1 in every 5 breast cancers contains cells with extra copies of the gene that makes the human epidermal growth factor 2 (HER2) protein.
These HER2 proteins look like thin spikes or antennas on the outer surface of a cell.
In healthy cells, HER2 proteins are far apart. So when a cell needs to divide, two of these HER2 proteins intentionally join together in a regulated, controlled way, signaling the cell to replicate.
However, when cells have higher than typical amounts of HER2 proteins, they can divide in an uncontrolled manner.
“If a cell is studded with all of these HER2 proteins, the proteins can bump into each other in a manner that is not well regulated,” says Dr. Leon-Ferre. “When they bump into each other unintentionally, they activate uncontrolled cell division.”
For this reason, HER2 positive breast cancers are considered more aggressive than HER2-negative cancers.
How is HER2 status determined?
To determine the HER2 status of your tumor, a small sample of breast tissue is usually removed. This is called a biopsy. A pathologist uses a colored stain that makes the HER2 proteins more visible. This test is called immunohistochemistry (IHC) and uses the numbers 0 to 3 to designate HER2 status. A score of 0 represents no detectable amount of HER2, and a score of 3 represents excessive amounts.
New HER2 categories
In the past, tumors in the category of 0 and 1 were considered HER2 negative, while tumors in the category of 3 were considered HER2 positive. Tumors that fell in the category of 2 were considered indeterminate. For those tumors, a second test called fluorescence in situ hybridization (FISH) was done to determine if they were HER2 positive or HER2 negative.
However, more recently, this classification system has broadened. A subset of tumors previously considered to be HER2 negative — but that have small amounts of HER2 protein — have been reclassified as HER2 low and HER2 ultralow.
| IHC test result | What it means | |
| 3+ | HER2 positive | |
| 2+ | Positive FISH test | HER2 positive |
| 2+ | Negative FISH test | HER2 low |
| 1+ | HER2 low | |
| >0 <1 | HER2 ultralow | |
| 0 | HER2 negative | |
How does HER2-low breast cancer differ from HER2-positive breast cancer?
As mentioned earlier, breast cancer experts once used only two designations — HER2 positive and HER2 negative — to describe a cancer’s HER2 status. Today, two additional designations, HER2 low and HER2 ultralow, are becoming more widely used. Here’s what the classifications mean.
HER2 positive
This status describes breast cancer cells with elevated HER2 protein levels. Because so many HER2 protein spikes populate these cancer cells, these breast cancers are considered more aggressive than HER2-negative cancers.
However, unlike HER2-negative breast cancers, HER2-positive cancers can be treated with a type of medication known as HER2-targeted therapy. This therapy encases HER2 proteins like soundproof armor, stopping them from touching and triggering uncontrolled cell division.
Read more: HER2-positive breast cancer: What can you expect?
HER2 negative
Under the new classification, HER2-negative breast cancer cells have no detectable amount of HER2 proteins. These breast cancers tend to be less aggressive than HER2-positive breast cancers. They also do not tend to respond to most HER2-targeted therapies.
HER2 low
More recently, scientists discovered that some breast cancers previously called HER2-negative cancers in fact have low levels of the HER2 protein. These cancer cells may still respond to a newer class of HER2-targeted therapies called antibody-drug conjugates (ADCs). ADCs work differently from the traditional targeted therapies used to treat HER2-positive breast cancer cells. Unlike the older targeted medicines, ADCs neutralize HER2 proteins in the following two ways:
- Like traditional HER2-targeted therapies, ADCs encase the HER2 protein.
- Unlike traditional HER2-targeted therapies, ADCs contain chemotherapy. When they attach to a HER2 protein, the cell ingests the chemotherapy and dies.
This second mechanism makes ADCs especially helpful in treating HER2-low breast cancer cells. Because these treatments also deliver chemotherapy to cells expressing the HER2 protein, they’re effective even on cancer cells with small amounts of HER2 protein.
HER2 ultralow
These breast cancer cells contain fewer HER2 proteins than do HER2-low breast cancer cells. However, they may still respond to ADC treatment.
How is HER2-low breast cancer treated?
To determine your treatment approach, you and your healthcare professional consider many factors, including your cancer’s type, stage, grade and tumor markers. If your cancer hasn’t spread beyond the breast, you’ll likely undergo surgery to remove the tumor, along with chemotherapy and radiation.
The Food and Drug Administration (FDA) has approved the use of newer ADC HER2-targeted medicines — such as trastuzumab deruxtecan (Enhertu) — for HER2-positive or HER2-low stage IV breast cancer, which is cancer that has spread (metastasized) to other parts of the body.
These newer therapies are delivered via an infusion. Potential side effects include an increased risk of lung disease. Because of this, your healthcare professional may monitor you for cough, shortness of breath, fever and other respiratory symptoms.
Research is underway to determine whether ADC therapy may also benefit people with the following breast cancer types and stages:
- Stage IV HER2-ultralow and HER2-negative breast cancers.
- Early-stage HER2-positive and HER2-low cancers that have not spread.
“We know that this new medication helps people with late-stage HER2-low breast cancer live longer,” says Dr. Leon-Ferre. “We haven’t proved yet whether this medication can cure cancer in the earlier stages, but those studies are ongoing.”
Prognosis for HER2-low breast cancer
Your HER2-low status likely won’t affect whether or how quickly your breast cancer spreads, says Dr. Leon-Ferre.
However, unlike HER2-negative cancer, the HER2-low designation provides your healthcare professional with an additional FDA-approved cancer-fighting tool should your cancer spread beyond the breast and lymph nodes.
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
Relevant reading
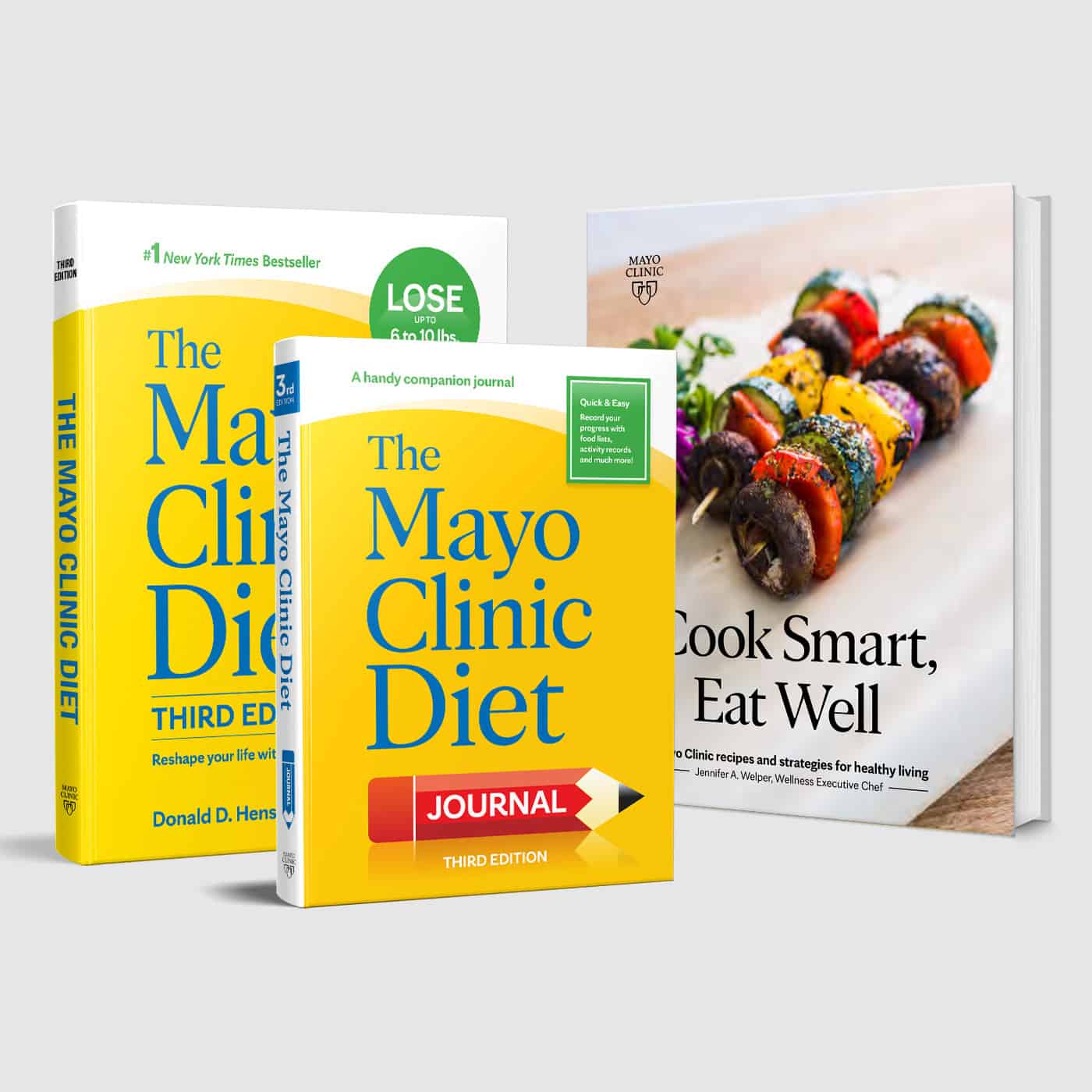
Mayo Clinic Diet and Cook Smart, Eat Well Bundle
This revised edition of the #1 New York Times bestselling book offers a simple, time-tested, no-nonsense approach to losing weight and keeping it off. The Mayo Clinic Diet by Donald D. Hensrud, M.D., isn’t a fad diet – it’s an approach that draws on years of research from thousands of individuals seeking…